Shortly before Cindy was removed from hospice they asked me whether beating the odds for keeping her alive was really what she would have wanted. They were questioning whether choosing quality of life measures over palliative care actually gave Cindy a life she wants to be living.
Three perspectives matter for choosing quality of life over palliative care measures. The day she received the official early onset diagnosis Cindy cried during the ride home, sad about the continued cognitive decline she faced. Once we got in the house she went into the attic to sort out what our daughters should inherit from her, now in gracious acceptance that she had effectively received an early death sentence. Cindy never feared death as much as becoming a burden. I admit that from the Cindy of the past perspective I made the wrong choice. If she could have viewed this future for us she would have requested I stop prolonging the inevitable.
From my perspective, Cindy’s main concern does not apply because she has not burdened me, and I am not trying to be a martyr. I knew that caregivers for patients with dementia are six times more likely to get dementia as well, and if that happened we were both doomed. I have been willing from the start to relinquish my caregiver duties if I started sensing my own cognitive decline, but my mind still is sharp … or at least I think so. 😉
The perspective that matters most is the hardest to gauge, the Cindy of the present. We humans have a marvelous ability to adapt to changing environments and conditions. Consider the spirit and joy of the participants in the Paralympic Games. A person may not want to be alive with no legs until they go through the experience and adapt. Can such adaptable spirit and joy be experienced as well when one has dementia?
My life as a caregiver for Cindy provides testimony to that. I posted on this blog about the time I suggested to Cindy, when we walked up ramps because of her balance problem with stairs, that we enter a marathon. She enthusiastically assented to the idea, perfectly oblivious to the impossibility. The Cindy of the past would know better, but knowing better does not matter for enjoying the present.
Before her first seizure and the start of hospice I detected moments of sadness and frustration in Cindy that, if prolonged, might have caused the Cindy of the past to scold me for doing my job well. Yet I always could make her smile at any time. Companions claimed they came just to see that smile. A smile as endearing as Cindy’s is not an attempt to put on a brave face, but an expression of the joy she feels. The Cindy of the past would cringe at seeing her future self having to be held up while we “danced,” but the Cindy of the present beamed.
Along this journey to live well in the face of tragedy, the Cindy of the present never confused herself with the Cindy of the past. Though she no longer could say names she never confused family members of the present with someone from her past. She never had episodes with living in the past, an occasional characteristic of dementia. Her mind stayed focused on the present, I suspect because she enjoyed herself more than the Cindy of the past imagined possible.
Once the hospice years started the smiles disappeared. Some companions still swore they detected a smile from her when they visited. Maybe that was wishful thinking on their part; maybe I am spoiled by the radiance of Cindy’s normal smile. What I still detect from Cindy are extended moments of peace in her countenance, along with sighs of contentment when I hold her in my lap.
From taking care of my mother at home with dementia I know what prolonged bouts of melancholy look like. I know what prolonged bouts of anguish look like. After my mother spent a few months in a nursing home I knew what permanent emptiness looked like. I do not detect any of this with Cindy. The Cindy of the past may abhor that she is still alive at this point, lasting even beyond hospice, but I do not think that is what the Cindy of the present feels yet.
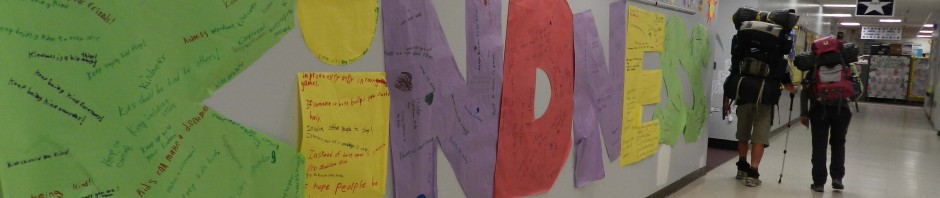
Kirk of the past could have learned from Cindy of the present. As we hiked across the country, our most amazing journey out of many, I apprehended a time when we would not be able to share those amazing memories. As we pursued our bucket list and Cindy was full of smiles, I apprehended when she would pass away and take those smiles with her. I am embarrassed to admit I started planning her memorial service in 2016, based on my mother’s rate of decline and the knowledge that early onset often proceeds rapidly.
Lesson learned. I focus on the present now with little apprehension about what the future brings. With a DNR in place, I leave to Cindy the decision of when I have done enough, trusting that I will not mistake her nonverbal signals when she feels her time has come to pass. Perhaps she will stop eating; perhaps she will look empty; perhaps she will look so distressed that morphine will be warranted. Whatever the signal, my guide will be Cindy of the present, not Cindy of the past.